Advances on the application of physical airway clearance techniques in the treatment of inhalation injury
-
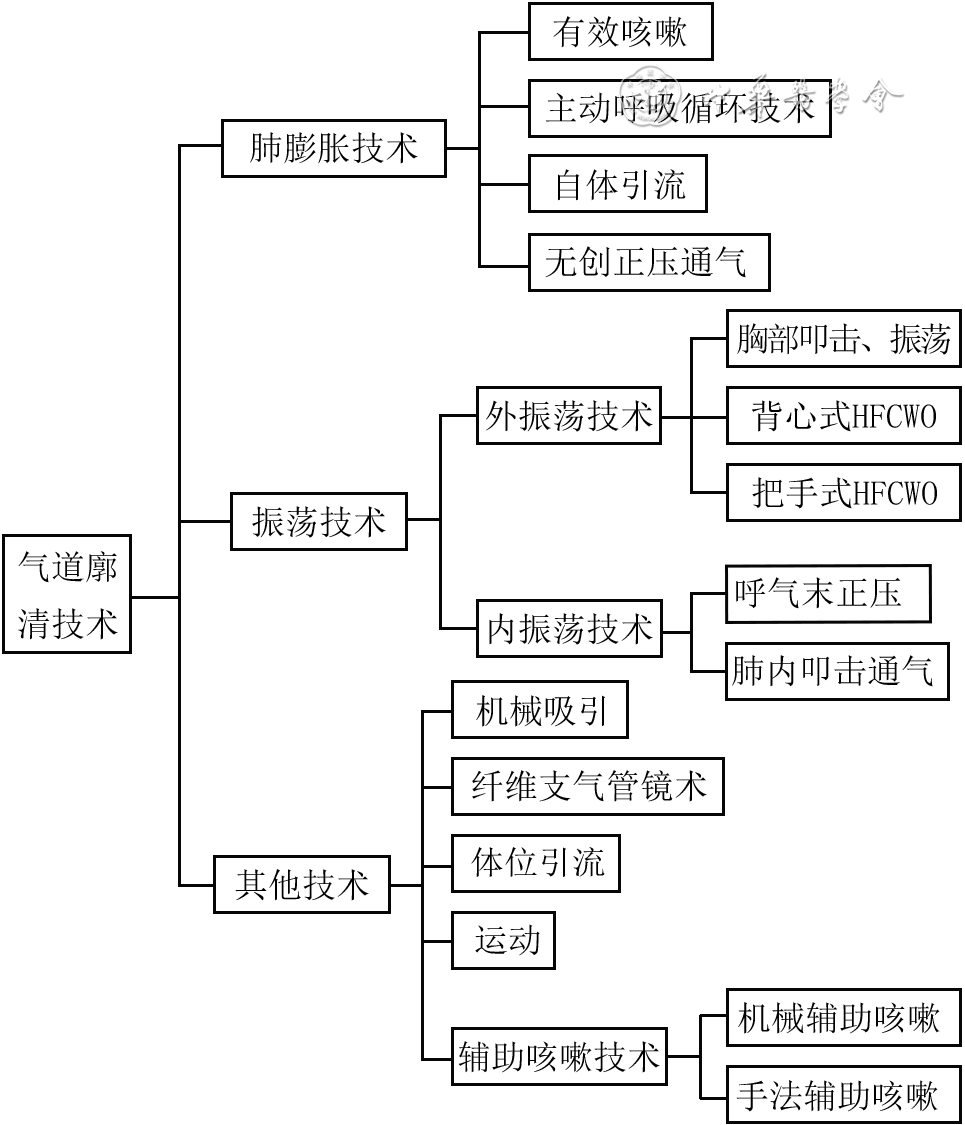
摘要: 尽管烧伤伴吸入性损伤患者的救治已经取得了很大成功,但从流行病学方面来看,吸入性损伤仍是目前群体性烧伤最常见的死亡因素,此类患者往往体表烧伤总面积较大,救治困难,其中气道管理是核心环节之一。物理性气道廓清技术(ACT)通过物理的方式作用于患者呼吸系统,使气道内的分泌物及异物排出,实现气道廓清,改善气体交换;此外,该技术还对诸多并发症具有防治或缓解作用,从而改善吸入性损伤患者的临床结局。该文就物理性ACT在吸入性损伤治疗领域的应用进行综述,为临床医护人员选择与患者病情相对应的物理性ACT提供决策依据。Abstract: Although the treatment of patients with burns combined with inhalation injury has achieved great success, from the perspective of epidemiology, inhalation injury is still the most common cause of death in mass burns. Such patients often suffered burns of large total body surface area, which is difficult to treat, with airway management as one of the core links. Physical airway clearance technique (ACT) acts on a patient's respiratory system by physical means, to discharge secretions and foreign bodies in the airway, achieve airway clearance, and improve gas exchange. In addition, the technique can prevent or alleviate many complications, thereby improving the clinical outcome of patients with inhalation injury. This article reviews the application of physical ACT in the field of inhalation injury, and to provide decision-making basis for clinical medical staff to choose physical ACT corresponding to the patient's condition.
-
Key words:
- Burns /
- Airway management /
- Inhalation injury /
- Phisical airway clearance techniques
-
参考文献
(40) [1] EdelmanDA, KhanN, KempfK, et al. Pneumonia after inhalation injury[J]. J Burn Care Res, 2007,28(2):241-246. DOI: 10.1097/BCR.0B013E318031D049. [2] 刘萌 12年严重烧伤患者流行病学特点及变化趋势 上海 上海交通大学 2018 31 32 刘萌. 12年严重烧伤患者流行病学特点及变化趋势[D].上海:上海交通大学,2018:31-32.
[3] MlcakRP, SumanOE, HerndonDN. Respiratory management of inhalation injury[J]. Burns, 2007,33(1):2-13. DOI: 10.1016/j.burns.2006.07.007. [4] VeeravaguA, YoonBC, JiangB, et al. National trends in burn and inhalation injury in burn patients: results of analysis of the nationwide inpatient sample database[J]. J Burn Care Res, 2015,36(2):258-265. DOI: 10.1097/BCR.0000000000000064. [5] 豆哲, 张国安. 系统综述我国烧伤患者吸入性损伤的流行病学特征[J] . 中华烧伤杂志, 2021, 37(7): 654-660. DOI: 10.3760/cma.j.cn501120-20200306-00129. [6] 程文凤 中国烧伤流行病学研究现状及多中心大面积烧伤患者流行病学调查分析 北京 中国人民解放军医学院 2017 程文凤.中国烧伤流行病学研究现状及多中心大面积烧伤患者流行病学调查分析[D].北京:中国人民解放军医学院,2017.
[7] 中国病理生理危重病学会呼吸治疗学组. 重症患者气道廓清技术专家共识[J/OL]. 中华重症医学电子杂志,2020,6(3):272-282[2022-06-08]. https://med.wanfangdata.com.cn/Paper/Detail?id=PeriodicalPaper_zhzzyxdzzz-wlb202003007&dbid=WF_QK. DOI: 10.3877/cma.j.issn.2096-1537.2020.03.007. [8] PenconekA, MichalczukU, SienkiewiczA, et al. The effect of desert dust particles on rheological properties of saliva and mucus[J]. Environ Sci Pollut Res Int, 2019,26(12):12150-12157. DOI: 10.1007/s11356-019-04628-x. [9] PuchelleE, ZahmJM, QuemadaD. Rheological properties controlling mucociliary frequency and respiratory mucus transport[J]. Biorheology, 1987,24(6):557-563. DOI: 10.3233/bir-1987-24606. [10] SheridanRL, SchaeferPW, WhalenM, et al. Case records of the Massachusetts General Hospital. Case 36-2012. Recovery of a 16-year-old girl from trauma and burns after a car accident[J]. N Engl J Med, 2012,367(21):2027-2037. DOI: 10.1056/NEJMcpc1200088. [11] MosierMJ, PhamTN. American Burn Association Practice guidelines for prevention, diagnosis, and treatment of ventilator-associated pneumonia (VAP) in burn patients[J]. J Burn Care Res, 2009,30(6):910-928. DOI: 10.1097/BCR.0b013e3181bfb68f. [12] 李国辉, 徐昌政, 吴燮卿, 等. 烧伤及合并吸入性损伤病人的肺功能检测[J].急诊医学,1998(5):303-305. [13] CaoL, ZhangXG, WangJG, et al. Pulmonary function test findings in patients with acute inhalation injury caused by smoke bombs[J]. J Thorac Dis, 2016,8(11):3160-3167. DOI: 10.21037/jtd.2016.11.94. [14] LamNN, HungTD. ARDS among cutaneous burn patients combined with inhalation injury: early onset and bad outcome[J]. Ann Burns Fire Disasters, 2019,32(1):37-42. [15] 朱峰. 吸入性损伤的临床诊断和防治对策[J].中华烧伤杂志,2018,34(5):293-296. DOI: 10.3760/cma.j.issn.1009-2587.2018.05.009. [16] 中国老年医学学会烧创伤分会. 吸入性损伤临床诊疗全国专家共识(2018版)[J].中华创伤杂志,2018,34(11):971-976. DOI: 10.3760/cma.j.issn.1001-8050.2018.11.003. [17] BachJR. Update and perspective on noninvasive respiratory muscle aids. Part 2: the expiratory aids[J]. Chest, 1994,105(5):1538-1544. DOI: 10.1378/chest.105.5.1538. [18] HasaniA, PaviaD, AgnewJE, et al. Regional mucus transport following unproductive cough and forced expiration technique in patients with airways obstruction[J]. Chest, 1994,105(5):1420-1425. DOI: 10.1378/chest.105.5.1420. [19] KuboT, OsukaA, KabataD, et al. Chest physical therapy reduces pneumonia following inhalation injury[J]. Burns, 2021,47(1):198-205. DOI: 10.1016/j.burns.2020.06.034. [20] 吴巍巍, 蔡夺, 迟骋, 等. 集束化气道管理在重度吸入性损伤气管切开患者气道护理中的应用[J].中华现代护理杂志,2017,23(34):4314-4318. DOI: 10.3760/cma.j.issn.1674-2907.2017.34.002. [21] ReperP, van LooyK. Chest physiotherapy using intrapulmonary percussive ventilation to treat persistent atelectasis in hypoxic patients after smoke inhalation[J]. Burns, 2013,39(1):192-193. DOI: 10.1016/j.burns.2012.04.015. [22] MillerAC, FerradaPA, KadriSS, et al. High-frequency ventilation modalities as salvage therapy for smoke inhalation-associated acute lung injury: a systematic review[J]. J Intensive Care Med, 2018,33(6):335-345. DOI: 10.1177/0885066617714770. [23] GuoB, BaiY, MaY, et al. Preclinical and clinical studies of smoke-inhalation-induced acute lung injury: update on both pathogenesis and innovative therapy[J]. Ther Adv Respir Dis, 2019,13:1753466619847901. DOI: 10.1177/1753466619847901. [24] AllanPF, HollingsworthMJ, ManiereGC, et al. Airway humidification during high-frequency percussive ventilation[J]. Respir Care, 2009,54(3):350-358. [25] OguraH, SumiY, MatsushimaA , et al. Smoke inhalation injury: diagnosis and respiratory management[J]. Nihon Geka Gakkai Zasshi, 2005, 106(12):740-744. [26] Edgar DW Group A Burn survivor rehabilitation: principles and guidelines for the Allied Health Professional Allied Health Forum Australian and New Zealand Burn Association (ANZBA) 2013 2007-03 2022-06-08 https://anzba.org.au/care/allied-health-guidelines/ EdgarDW, GroupA. Burn survivor rehabilitation: principles and guidelines for the Allied Health Professional Allied Health Forum Australian and New Zealand Burn Association (ANZBA)[EB/OL]. 2013:73.(2007-03)[2022-06-08].https://anzba.org.au/care/allied-health-guidelines/.
[27] FrownfelterD, DeanE. Cardiovascular and pulmonary physical therapy evidence to prACTice[M]. 6th ed. St Louis: Elsevier, 2022:324e7. [28] 王淑君,申传安,李菊清,等. 大面积烧伤合并吸入性损伤患者气管切开术后吸痰的护理[J]. 中华现代护理杂志,2013,19(31):3873-3875. DOI: 10.3760/cma.j.issn.1674-2907.2013.31.019. [29] HassanZ, WongJK, BushJ, et al. Assessing the severity of inhalation injuries in adults[J]. Burns, 2010,36(2):212-216. DOI: 10.1016/j.burns.2009.06.205. [30] 吴抽浪, 周丽春, 崔可, 等. 早期纤维支气管镜灌洗联合机械通气治疗重度吸入性损伤八例[J].中华烧伤杂志,2015,31(1):64-65. DOI: 10.3760/cma.j.issn.1009-2587.2015.01.017. [31] 蒋南红,王德运,席毛毛,等.纤维支气管镜气道灌洗治疗特重度烧伤合并重度吸入性损伤患者的回顾性研究[J].中华烧伤杂志,2020,36(4):252-259. DOI: 10.3760/cma.j.cn501120-20191203-00451. [32] CarrJA, CrowleyN. Prophylactic sequential bronchoscopy after inhalation injury: results from a three-year prospective randomized trial[J]. Eur J Trauma Emerg Surg, 2013,39(2):177-183. DOI: 10.1007/s00068-013-0254-x. [33] TonelliAR, ZeinJ, AdamsJ, et al. Effects of interventions on survival in acute respiratory distress syndrome: an umbrella review of 159 published randomized trials and 29 meta-analyses[J]. Intensive Care Med, 2014,40(6):769-787. DOI: 10.1007/s00134-014-3272-1. [34] HaleDF, CannonJW, BatchinskyAI, et al. Prone positioning improves oxygenation in adult burn patients with severe acute respiratory distress syndrome[J]. J Trauma Acute Care Surg, 2012,72(6):1634-1639. DOI: 10.1097/TA.0b013e318247cd4f. [35] 中国老年医学学会烧创伤分会, 中华医学会烧伤外科学分会重症学组. 成人烧伤俯卧位治疗全国专家共识(2022版)[J].中华烧伤与创面修复杂志,2022,38(7):601-609. DOI: 10.3760/cma.j.cn501120-20211208-00407. [36] PalackicA, SumanOE, PorterC, et al. Rehabilitative exercise training for burn injury[J]. Sports Med, 2021,51(12):2469-2482. DOI: 10.1007/s40279-021-01528-4. [37] WonYH, ChoYS, JooSY, et al. The effect of a pulmonary rehabilitation on lung function and exercise capacity in patients with burn: a prospective randomized single-blind study[J]. J Clin Med, 2020, 9(7):2250. DOI: 10.3390/jcm9072250. [38] KnudtzenFC, SprehnM, VestboJ, et al. Mechanical insufflation/exsufflation compared with standard of care in patients with pneumonia: a randomised controlled trial[J]. Eur J Anaesthesiol, 2020,37(11):1077-1080. DOI: 10.1097/EJA.0000000000001209. [39] 徐剑锋, 郭芝廷, 毛越, 等. 集束化呼吸治疗在烧伤合并中重度吸入性损伤患者气道管理中的应用[J].中华烧伤杂志,2015,31(2):140-142. DOI: 10.3760/cma.j.issn.1009-2587.2015.02.016. [40] AliZA, EladlHM, AbdelbassetWK, et al. Inhalation injury in adult males: evaluation of the short-term efficacy of transcutaneous electrical acupoint stimulation on pulmonary functions and diaphragmatic mobility after burn: a double-blind randomized controlled study[J]. Burns, 2022, 48(8):1933-1939. DOI: 10.1016/j.burns.2022.01.015. -








 下载:
下载: