Clinical effects of free superficial peroneal artery perforator flaps in repairing skin and soft tissue defects of the hallux
-
摘要:
目的 探讨游离腓浅动脉穿支皮瓣修复拇趾皮肤软组织缺损的临床效果。 方法 采用回顾性观察性研究方法。2020年1月—2021年1月,苏州大学附属瑞华医院足踝外科收治13例符合入选标准的拇趾皮肤软组织缺损患者,其中男12例、女1例,年龄16~53岁。术前于患趾同侧小腿行彩色多普勒超声定位腓浅动脉穿支穿出点并于体表标记。手术于脊椎麻醉+连续硬膜外麻醉下进行,扩创后皮肤软组织缺损面积为4.5 cm×2.5 cm~12.0 cm×3.0 cm。根据创面的大小、形状,以腓骨小头与外踝尖连线向胫侧平移2 cm为皮瓣轴心线,以轴心线中点附近穿支穿出点为中心,设计腓浅动脉穿支皮瓣。皮瓣切取面积为5.0 cm×3.0 cm~13.0 cm×4.0 cm,游离蒂部时切取部分深筋膜。供区创面直接缝合。术中记录穿支数目、类型及皮瓣切取时间,测量穿支血管蒂长度及穿支直径。术后记录皮瓣成活情况、供受区愈合时间及愈合情况。随访记录皮瓣的色泽、质地、弹性,患者站立及行走功能,供区恢复情况以及患者对供受区恢复情况的满意度。末次随访,采用英国医学研究会感觉功能评定标准评定皮瓣感觉,采用美国足踝外科学会评分系统评价患肢功能并计算优良率。 结果 术中共探及腓浅动脉穿支13条,均为肌间隔穿支,穿支直径0.3~0.5 mm;血管蒂长度2~5 cm。皮瓣切取时间11~26 min。13例患者术后皮瓣均完全成活。术后9~18 d,供受区创面均愈合良好。随访6~14个月,皮瓣色泽、质地、弹性良好;11例患者外形无明显臃肿,另外2例患者因外观臃肿,Ⅱ期行皮瓣修薄整形;所有患者均恢复正常行走、站立功能;供区仅遗留一条线状瘢痕,无明显瘢痕增生或色素沉着;所有患者对供受区恢复情况表示满意。末次随访,皮瓣感觉功能评定为S3级者2例、S2级者9例、S1级者2例;患肢功能评定为优者7例、良者6例,优良率为100%。 结论 游离腓浅动脉穿支皮瓣血管解剖较为恒定,皮瓣薄且耐磨,皮瓣切取后供区损伤小,可以最大限度保留拇趾外形及功能,是一种修复拇趾皮肤软组织缺损的有效方法。 Abstract:Objective To explore the clinical effects of free superficial peroneal artery perforator flaps in repairing skin and soft tissue defects of the hallux. Methods A retrospective observational study was conducted. From January 2020 to January 2021, 13 patients with skin and soft tissue defects of the hallux who met the inclusion criteria were admitted to Department of Foot and Ankle Surgery of Ruihua Affiliated Hospital of Soochow University, including 12 males and 1 female, aged 26 to 53 years. Before operation, the perforating point of the superficial peroneal artery perforator was located by color Doppler ultrasound on the calf on the same side of the affected hallux and marked on the body surface. The operation was performed under spinal anesthesia combined with continuous epidural anesthesia. The area of skin and soft tissue defect after debridement was 4.5 cm×2.5 cm to 12.0 cm×3.0 cm. According to the size and shape of the wound, the superficial peroneal artery perforator flap was designed with the line between the fibular head and the lateral malleolus tip parallel shifting 2 cm to the tibial side as the flap axis line, and the perforating point of the perforator near the midpoint of the axis line as the center. The cut area of the flap was 5.0 cm×3.0 cm to 13.0 cm×4.0 cm, and part of the deep fascia was cut when the pedicle was freed. The donor site wound was sutured directly. During the operation, the number and type of the perforator and the cutting time of the flap were recorded, and the length of the perforator pedicle and diameter of the perforator were measured. The survival of the flap, the healing time and the healing condition of the donor and recipient areas were recorded after operation. The color, texture, elasticity of the flap, standing and walking functions of patients, the recovery of the donor area, and the patients' satisfaction with the recovery of the donor and recipient areas were recorded during the follow-up. At the last follow-up, the sensation of the flap was evaluated by the British Medical Association sensory function evaluation standard, the function of the affected limb was evaluated by the American Society of Foot and Ankle Surgery scoring system, and the excellent and good rate of the function of the affected limb was calculated. Results A total of 13 perforators of the superficial peroneal artery were detected during the operation, all of which were septocutaneous perforators, and the perforator diameter was 0.3 to 0.5 mm. The vascular pedicle length was 2 to 5 cm. Flap cutting time was 11 to 26 minutes. The flaps of 13 patients all survived completely. The wounds at the donor and recipient sites healed well 9 to 18 days after operation. During follow-up of 6 to 14 months, the flaps had good color, texture, and elasticity; 11 patients had no obvious bloated appearance, and the other 2 patients underwent flap thinning and plastic surgery in the second stage because of their bloated appearance; all the patients returned to normal walking and standing functions. There was only one linear scar left in the donor site, with no obvious scar hyperplasia or hyperpigmentation. All the patients were satisfied with the recovery of the donor and recipient areas. At the last follow-up, the sensation of the flap was evaluated as grade S3 in 2 cases, grade S2 in 9 cases, and grade S1 in 2 cases; the function of the affected limb was evaluated as excellent in 7 cases and good in 6 cases, with an excellent and good rate of 100%. Conclusions The free superficial peroneal artery perforator flap has relatively constant vascular anatomy, which is thin and wear-resistant, with less damage to the donor site after flap excision, and can preserve the shape and function of the hallux to the greatest extent. It is an effective method for repairing skin and soft tissue defect of the hallux. -
(1)腓浅动脉穿支解剖位置较为恒定,均走行于肌间隔内,无须过多解剖游离,转移不受蒂部旋转角度限制,供区损伤小,是修复拇趾皮肤软组织缺损较为理想的供区,此前鲜见报道。
(2)术前于腓骨小头与外踝尖连线向胫侧平移2 cm周围行彩色多普勒超声定位腓浅动脉穿支,穿支定位更明确,操作难度、手术风险明显降低。
随着工业的飞速发展,外伤所致拇趾皮肤软组织缺损患者日益增多,以往多行残端修整或截趾,以牺牲趾体长度的代价来换取创面的简单闭合。但由于生活水平的提高,患者保留拇趾长度、恢复良好外观及功能的意愿愈发强烈,临床医师处理愈发棘手[1, 2]。本研究团队采用游离腓浅动脉穿支皮瓣修复拇趾皮肤软组织缺损,临床效果较佳。
1. 对象与方法
本回顾性观察性研究符合《赫尔辛基宣言》的基本原则。
1.1 入选标准
纳入标准:拇趾皮肤软组织缺损,采用游离腓浅动脉穿支皮瓣修复者;双侧小腿皮肤完整,且无外伤史及皮肤病史者。排除标准:随访时间不足6个月者,术中及随访资料不全者。
1.2 临床资料
2020年1月—2021年1月,苏州大学附属瑞华医院足踝外科收治13例拇趾皮肤软组织缺损患者,其中男12例、女1例;年龄16~53岁,平均41岁。致伤原因:重物砸伤者6例,叉车压伤者3例,皮带绞伤者1例,机器夹伤者2例,电锯伤者1例。患者伤后1~4 h,平均2.5 h急诊入院。入院后完善相关检查,均行急诊Ⅰ期清创,伴骨折行骨折复位内固定术者13例,伴血管、神经、肌腱损伤行探查修复术者2例,趾体离断行断趾再植术者5例,皮肤撕脱行撕脱皮肤回植术者6例。急诊术后皮肤软组织坏死部位:拇趾甲床者4例,拇趾背侧者4例,拇趾趾腹者3例,拇趾腓侧者1例,拇趾胫侧者1例。待坏死界限清晰后,行游离腓浅动脉穿支皮瓣修复。急诊手术至皮瓣修复时间为10~38 d,平均19.5 d。
1.3 治疗方法
1.3.1 术前穿支定位
术前于患趾同侧小腿,应用彩色多普勒超声诊断仪,沿腓骨小头至外踝尖连线向胫侧平移2 cm的线,由近及远寻找腓浅动脉穿支穿出点并于体表标记。测量腓骨小头与外踝尖连线长度(32~37 cm,平均34 cm)并标记中点。13例患者13个皮瓣供区共定位41条穿支,平均每个供区3.15条穿支。
1.3.2 麻醉方式
所有手术均采用脊椎麻醉+连续硬膜外麻醉。
1.3.3 受区准备
供受区均在气压止血带下进行手术。予体积分数3%过氧化氢、生理盐水、10 g/L苯扎溴铵冲洗创面,彻底切除坏死组织,刮除创面肉芽组织直至出现新鲜渗血,修剪距创缘0.2 cm的创周皮肤。部分患者见拇趾末节趾骨部分坏死,予摘除死骨。用生理盐水再次冲洗创面后,自创缘纵行切开皮肤,解剖受区血管,首选第一跖背动脉及趾背静脉为受区血管。放松止血带,观察血管喷血良好后标记备用。本组患者扩创后皮肤软组织缺损面积为4.5 cm×2.5 cm~12.0 cm×3.0 cm。
1.3.4 皮瓣设计
根据创面大小、形状设计样布。将腓骨小头至外踝尖连线向胫侧平移2 cm的线作为皮瓣轴心线,以轴心线中点附近术前彩色多普勒超声定位的穿支穿出点为中心,根据样布设计腓浅动脉穿支皮瓣,皮瓣面积较创面面积适当扩大。
1.3.5 皮瓣切取
沿设计线切开皮瓣前缘皮肤,于深筋膜浅层解剖寻找腓浅动脉穿支穿出点。确认穿支进入皮瓣后,根据穿支实际位置,适当调整皮瓣的切取位置。游离皮瓣周缘,于腓骨长肌和趾长伸肌间隔内,沿穿支走行向近端解剖分离,沿途结扎穿支发出的肌支,直至见到腓浅动脉主干及其伴行的腓浅神经并加以保护。解剖皮瓣蒂部时,常规切取部分深筋膜,避免裸化蒂部穿支。根据受区需要,解剖出足够长度的血管蒂,予结扎并切断。本组患者皮瓣切取面积为5.0 cm×3.0 cm~13.0 cm×4.0 cm。将皮瓣转移至受区,与创缘缝合数针固定。供区彻底止血后直接缝合。
1.3.6 血管吻合
显微镜下将皮瓣蒂部血管与受区动静脉进行端端吻合。本组患者中,皮瓣蒂部血管与第一跖背动脉及趾背静脉吻合者10例,与足底内侧动脉及跖底静脉吻合者1例,与拇趾腓侧趾固有动脉及趾背静脉吻合者2例。皮瓣表面做一小切口观察皮瓣血运,松止血带见皮瓣血运佳后,缝合创缘。用无菌敷料包扎,医用高分子夹板外固定。
1.3.7 术后处理
补充血容量;常规行抗炎、抗凝、抗痉挛治疗;患肢抬高,略高于心脏水平;60 W烤灯照射;皮瓣表面切口处用肝素浸润的棉球湿敷。
1.4 观测指标
术中记录穿支数目、类型及皮瓣切取时间,测量皮瓣穿支血管蒂长度及穿支直径。术后记录皮瓣成活情况、供受区愈合时间及愈合后情况。随访记录皮瓣的色泽、质地、弹性,患者站立、行走功能,供区恢复情况以及患者对供受区恢复情况的满意度。末次随访,采用英国医学研究会感觉功能评定标准[3]评定皮瓣感觉功能,分为5级:S0级为感觉完全丧失,S1级为存在深部痛觉,S2级为存在浅感觉及触觉且有较弱的两点辨别觉,S3级为存在浅感觉及触觉且有较强的两点辨别觉,S4级为感觉正常;采用美国足踝外科学会评分系统[4]对患肢功能进行综合评价,满分为100分,其中90~100分为优,75~89分为良,50~74分为可,<50分为差,另计算优良率。
2. 结果
术中共探及腓浅动脉穿支13条,均为肌间隔穿支;血管蒂长度2~5 cm,平均4 cm;穿支直径0.3~0.5 mm,平均0.4 mm。皮瓣切取时间11~26 min,平均17 min。本组13例患者术后皮瓣均完全成活,未发生血管危象。术后9~18 d,平均13.7 d,供受区创面均愈合良好。术后随访6~14个月,平均8个月,皮瓣色泽、质地、弹性良好;11例患者外形无明显臃肿,另外2例患者因皮下脂肪较厚,外观臃肿,Ⅱ期行皮瓣修薄整形;所有患者均恢复正常行走、站立功能;小腿供区仅遗留一条线状瘢痕,无明显瘢痕增生或色素沉着;所有患者对供受区恢复情况表示满意。末次随访,皮瓣感觉功能评定为S3级者2例、S2级者9例、S1级者2例;患肢功能评分为81~97分,平均89.8分,其中评定为优者7例、良者6例,优良率为100%。
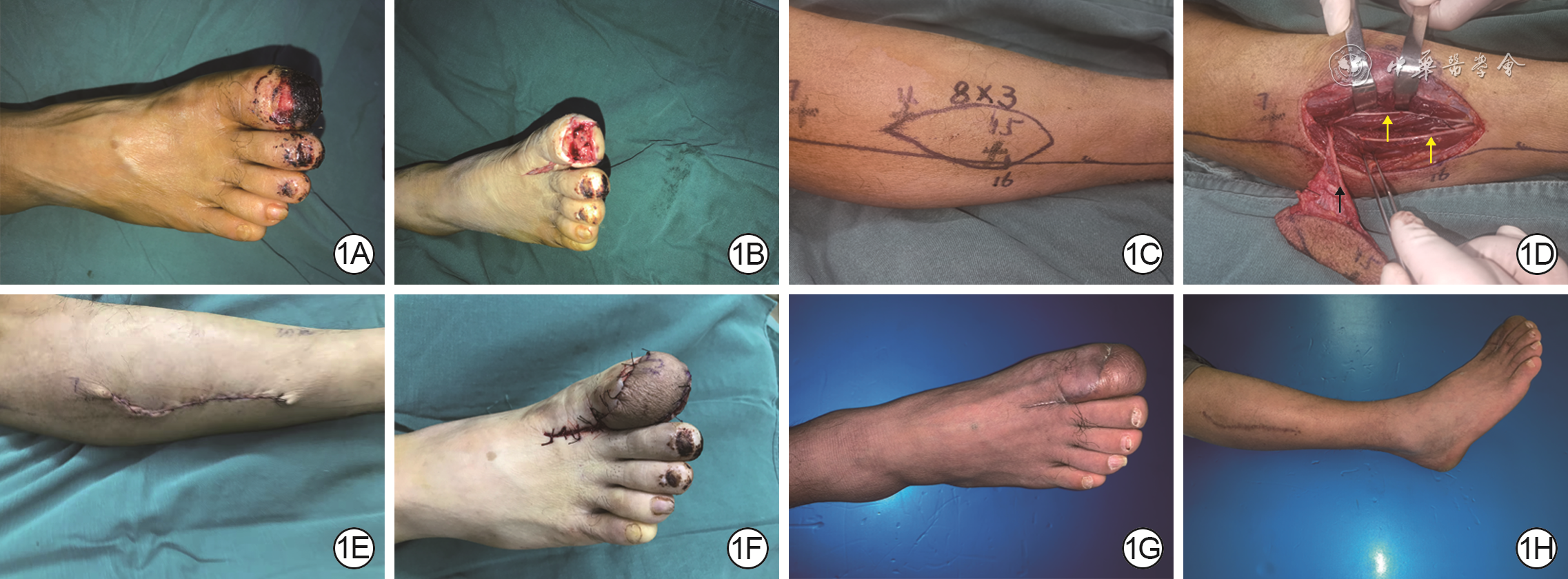
典型病例:患者男,52岁,因重物砸伤致右足拇趾末节骨折伴趾尖动脉、神经断裂及皮肤软组织挫裂3 h入院。入院后急诊行骨折复位内固定及血管、神经修复。术后7 d右足拇趾末节甲床处皮肤发黑、血运不佳,继续予换药观察。待坏死界限清晰后,于入院后12 d切取游离腓浅动脉穿支皮瓣修复创面。术前作右小腿腓骨小头与外踝尖连线,并向胫侧平移2 cm,于该连线周围行彩色多普勒超声定位穿支穿出点,并于体表标记。术前测量的腓骨小头与外踝尖连线长度为32 cm,标记其中点。术中扩创后创面面积为7.5 cm×2.5 cm。同前设计及切取面积为8.0 cm×3.0 cm的腓浅动脉穿支皮瓣,皮瓣血管蒂长度为5 cm、穿支直径为0.4 mm。皮瓣切取时间为11 min。皮瓣切取后供区直接缝合。将皮瓣蒂部血管与受区第一跖背动脉及趾背静脉端端吻合。术后皮瓣存活良好,未出现血管危象。术后10 d,供受区创面愈合。术后8个月随访,皮瓣色泽、质地、弹性良好,外形无明显臃肿;患者恢复正常行走、站立功能;供区仅遗留一条线状瘢痕,无明显瘢痕增生或色素沉着;患者对术后供受区恢复情况表示满意;皮瓣感觉恢复至S2级;患肢功能评分为97分,评定为优。见图1。
3. 讨论
拇趾在足部生物力学中起着至关重要的作用,其不仅参与步态周期的发起[5],同时还承担着行走过程中足趾60%的负荷[2]。大部分截趾或残端修整操作会损伤第一跖趾关节,使足胫侧负重功能受损,负重区域向前足腓侧转移,导致转移性跖痛或外侧足趾畸形[6]。拇趾解剖学完整性遭到破坏,足部抓持力、蹬地力减弱,长此以往,会导致足底溃疡及胼胝体形成。目前针对拇趾皮肤软组织缺损的修复,常需保留趾体长度,恢复解剖学完整性,实现可靠而美观的皮瓣覆盖的同时,将供区并发症降至最低,这也是目前临床医师追求的目标[7]。保留拇趾长度,不仅有利于恢复拇趾及其周围结构的解剖学完整性,还可满足患者对足部美观的要求,避免造成不良的心理影响。
针对拇趾皮肤软组织缺损,皮瓣供区选择较多,但各有优劣。带蒂皮瓣[8, 9, 10]无须显微外科操作,临床应用较广泛。为尽可能降低供区损伤,多于足部非功能区切取皮瓣[11, 12, 13, 14, 15, 16];部分学者选择皮神经营养血管皮瓣[17, 18, 19]以促进皮瓣感觉恢复。穿支皮瓣因较薄,不损伤供区主干血管,已被用于修复足部皮肤软组织缺损[20, 21, 22, 23]。随着显微外科技术的飞速发展,临床医师追求实现供瓣区美学缝合的同时,尽可能降低供区损伤[24, 25, 26, 27]。足部带蒂皮瓣虽与创面质地更为接近,但供受区位于同一部位,影响美观。皮瓣切取宽度有限,若切取面积较大,常需植皮修复,不美观亦不耐磨。小腿远端带蒂皮瓣虽无须进行显微吻合,但若皮瓣蒂部处理不当,易造成牵拉扭转,不利于皮瓣成活。
采用游离腓浅动脉穿支皮瓣修复拇趾皮肤软组织缺损,皮瓣血供丰富,穿支直径大部分为0.5 mm[28, 29, 30],与受区血管直径相近,供受区血管吻合后,皮瓣坏死鲜有发生[31, 32, 33, 34, 35, 36]。本研究术中测量的穿支直径平均0.4 mm,术后皮瓣均顺利成活,未发生血管危象。腓浅动脉穿支皮瓣供区位于小腿外侧,手术体位摆放方便,且该部位皮肤薄且耐磨,颜色、质地与足部接近,术后一般无须进行皮瓣修薄整形,本组也仅有2例患者因外形臃肿行皮瓣修薄整形。腓浅动脉穿支皮瓣蒂部均为肌间隔穿支,解剖游离操作简单,不损伤供区主干血管和肌肉组织;皮瓣血管蒂长度充足,可根据受区需要较为自由进行断蒂;皮瓣切取宽度小于4.0 cm,供区均可直接闭合,避免了因植皮对供区外观及功能的影响。本组患者术中大多选择第一跖背动脉与皮瓣蒂部血管吻合,无须牺牲受区主干血管即可重建皮瓣血运。另外,皮瓣切取时,可携带部分小腿深筋膜或腓骨长肌,用于修复伴有肌腱、肌肉等组织缺损或形成空腔的复杂创面。
但本术式存在以下不足:(1)穿支血管细,解剖费时费力;受区吻合时,操作难度大,有时无法进行端端吻合,对术者穿支血管解剖分离及显微外科技术要求高;(2)腓浅神经上段仅为过路神经,没有发出皮支进入皮瓣内[37],无法与受区合适神经吻合。术后皮瓣未恢复保护性感觉前,应注意防护,避免发生烫伤、冻伤等二次损伤。但因本组患者皮瓣切取面积较小,随访观察到患者术后6个月均可恢复保护性感觉,2例患者感觉甚至可恢复至S3级。
本术式注意事项:(1)术前以腓骨小头与外踝尖连线向胫侧平移2 cm为皮瓣轴心线,于轴心线周围行彩色多普勒超声定位穿支穿出点并于体表标记。优先以皮瓣轴心线中点附近穿支穿出点为中心设计皮瓣,根据术中实际情况对皮瓣位置进行适当调整。(2)优先选择第一跖背动脉作为受区动脉;当第一跖背动脉细小或缺如时,选择趾底动脉或足背动脉分支为受区动脉。本组患者中有3例第一跖背动脉缺如,皮瓣蒂部血管与足底内侧动脉相吻合者1例,与拇趾腓侧趾固有动脉相吻合者2例。(3)术中解剖时,不提倡裸化穿支,应携带部分深筋膜,保护穿支血管的同时,还可保留深筋膜中丰富的血管网。(4)血管吻合应尽量行端端吻合。当受区血管直径为皮瓣蒂部血管直径的2倍及以内时,可对蒂部血管行“鱼嘴样”处理,扩大外径后再吻合;当受区血管直径为皮瓣蒂部血管直径的2倍以上时,可携带一段腓浅动脉主干来进行吻合或将受区血管直径缩小的同时对蒂部血管行“鱼嘴样”处理。(5)皮瓣切取时要注意保护腓浅神经,以免其损伤导致小腿外侧及足背感觉功能障碍。
综上所述,游离腓浅动脉穿支皮瓣血管解剖较为恒定,皮瓣薄且耐磨,色泽、质地良好,皮瓣切取后供区损伤小,可以最大限度保留拇趾外形及功能,是一种修复拇趾皮肤软组织缺损的有效方法。
张韬:酝酿和设计研究、手术实施、采集资料、分析数据与论文撰写;柳志锦、刘胜哲:手术实施、采集资料、分析数据与修改文章;程俊楠、杨林:手术实施与采集资料;周荣、郭礼平、杨亮:手术实施与采集资料;熊胜:采集资料;巨积辉:酝酿和设计研究、手术实施、分析数据、修改文章与获取研究经费所有作者均声明不存在利益冲突 -
参考文献
(37) [1] LimthongthangR,EamsobhanaP.First dorsal metatarsal artery perforator flap to cover great toe defect[J].J Orthop Surg (Hong Kong),2017,25(3):2309499017739497.DOI: 10.1177/2309499017739497. [2] LeeY,LeeYH,KimMB,et al.The innervated distally based first dorsal metatarsal artery flap with a wide pedicle for reconstruction of a great toe defect[J].Clin Orthop Surg,2019,11(3):325-331.DOI: 10.4055/cios.2019.11.3.325. [3] NikiH,AokiH,InokuchiS,et al.Development and reliability of a standard rating system for outcome measurement of foot and ankle disorders I: development of standard rating system[J].J Orthop Sci,2005,10(5):457-465.DOI: 10.1007/s00776-005-0936-2. [4] KitaokaHB,AlexanderIJ,AdelaarRS,et al.Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes[J].Foot Ankle Int,1994,15(7):349-353.DOI: 10.1177/107110079401500701. [5] ChanJK,SongM,ShirleyR,et al.Free dorsal toe flap for reconstruction of the hallux[J].Plast Reconstr Surg Glob Open,2020,8(9):e3117.DOI: 10.1097/GOX.0000000000003117. [6] BargA,HarmerJR,PressonAP,et al.Unfavorable outcomes following surgical treatment of hallux valgus deformity: a systematic literature review[J].J Bone Joint Surg Am,2018,100(18):1563-1573.DOI: 10.2106/JBJS.17.00975. [7] ZeidermanMR, PuLLQ. Contemporary approach to soft-tissue reconstruction of the lower extremity after trauma[J/OL]. Burns Trauma, 2021,9:tkab024[2022-07-06]. https://pubmed.ncbi.nlm.nih.gov/34345630/.DOI: 10.1093/burnst/tkab024. [8] 李攀登,沈国良.携带腓肠肌的腓动脉穿支腓肠神经营养血管双血供复合组织瓣修复足踝部腔隙性缺损的临床效果[J].中华烧伤杂志,2019,35(5):392-394.DOI: 10.3760/cma.j.issn.1009-2587.2019.05.013. [9] 李海,张程,邓呈亮,等.腓动脉中低位穿支皮瓣带蒂转移修复足踝部皮肤软组织缺损的临床效果[J].中华烧伤杂志,2017,33(10):607-610.DOI: 10.3760/cma.j.issn.1009-2587.2017.10.004. [10] 秦建忠,朱振华,周聚普,等.腓动脉外踝前终末穿支降支蒂岛状皮瓣修复中足和前足软组织缺损[J].中华显微外科杂志,2020,43(1):20-23.DOI: 10.3760/cma.j.issn.1001-2036.2020.01.016. [11] 曹胜军,丰波,王凌峰,等.足底内侧岛状皮瓣修复足底负重区创面11例[J].中华烧伤杂志,2017,33(7):455-457.DOI: 10.3760/cma.j.issn.1009-2587.2017.07.016. [12] 黎斌,徐长春,刘志强,等.足内侧远端筋膜蒂岛状皮瓣修复(拇)趾创面缺损[J].中华手外科杂志,2016,32(1):73-74.DOI: 10.3760/cma.j.issn.1005-054X.2016.01.031. [13] 杨英才,李养群,叶永奇,等.(拇)横动脉分支皮瓣修复(拇)趾皮肤缺损[J].中华整形外科杂志,2017,33(3):224-225.DOI: 10.3760/cma.j.issn.1009-4598.2017.03.015. [14] 王国伟,王静,焦玉坤,等.逆行第1跖背动脉皮瓣在(足母)趾软组织缺损中的应用[J].中华显微外科杂志,2019,42(3):282-284.DOI: 10.3760/cma.j.issn.1001-2036.2019.03.019. [15] 张海永,王宝英,牛军,等.跗外侧动脉皮瓣修复足拇趾末节皮肤软组织缺损13例[J].郑州大学学报(医学版),2017,52(2):223-225.DOI: 10.13705/j.issn.1671-6825.2017.02.030. [16] 裴少琨,李卫海,崔留超,等.不同形式足内侧皮瓣修复前足软组织缺损[J].中国美容整形外科杂志,2019,30(11):651-654.DOI: 10.3969/j.issn.1673-7040.2019.11.004. [17] 李楚炎,李文庆,姚海波,等.足内侧皮神经营养血管远端蒂皮瓣修复前足软组织缺损[J].中国临床解剖学杂志,2017,35(4):445-447.DOI: 10.13418/j.issn.1001-165x.2017.04.018. [18] 杨洪涛,齐杰,李雯,等.足背内侧皮神经内侧支皮瓣修复足拇趾电击伤创面[J].中国美容整形外科杂志,2016,27(10):616-618.DOI: 10.3969/j.issn.1673-7040.2016.10.012. [19] 窦金兰,田振欣,郑珊珊,等.三维CT血管造影辅助设计足内侧隐神经营养血管皮瓣修复足远端软组织缺损[J].中华整形外科杂志,2020,36(2):175-179.DOI: 10.3760/cma.j.issn.1009-4598.2020.02.012. [20] 胡长青,连勇,白晓亮,等.游离胸背动脉穿支皮瓣修复小腿远端及足踝部创面九例[J].中华烧伤杂志,2018,34(4):240-242.DOI: 10.3760/cma.j.issn.1009-2587.2018.04.009. [21] 潘冬经,姚志伟,姜魏,等.腓肠内侧动脉穿支皮瓣修复四肢及面部皮肤软组织缺损六例[J].中华烧伤杂志,2017,33(12):772-775.DOI: 10.3760/cma.j.issn.1009-2587.2017.12.010. [22] 董建峰,史光华,王建国,等.游离腓肠内侧动脉穿支皮瓣修复(足母)𧿹甲瓣供区创面七例[J].中华显微外科杂志,2019,42(3):300-302.DOI: 10.3760/cma.j.issn.1001-2036.2019.03.027. [23] 胡朝波,邱勋永,林晶,等.腓动脉穿支皮瓣游离移植修复前足皮肤缺损13例[J].中华显微外科杂志,2017,40(5):486-488.DOI: 10.3760/cma.j.issn.1001-2036.2017.05.019. [24] 杜伟力,沈余明,胡骁骅,等.供瓣区美学修复方法的探讨[J].中华烧伤杂志,2020,36(2):97-105.DOI: 10.3760/cma.j.issn.1009-2587.2020.02.004. [25] 韩军涛,王洪涛,谢松涛,等.供瓣区选择与修复策略的初步探讨[J].中华烧伤杂志,2020,36(2):85-90.DOI: 10.3760/cma.j.issn.1009-2587.2020.02.002. [26] 刘毅.重视供区的美容修复[J].中华烧伤杂志,2020,36(2):81-84.DOI: 10.3760/cma.j.issn.1009-2587.2020.02.001. [27] 陈珺,章一新.章氏超减张缝合在闭合高张力创面中的临床应用效果[J].中华烧伤杂志,2020,36(5):339-345.DOI: 10.3760/cma.j.cn501120-20200314-00163. [28] YangX,ZhangG,LiuY,et al.Vascular anatomy and clinical application of anterolateral leg perforator flaps[J].Plast Reconstr Surg,2013,131(4):534e-543e.DOI: 10.1097/PRS.0b013e3182827675. [29] 秦向征,刘鹏,许东元,等.腓浅动脉皮支链的应用解剖[J].中华显微外科杂志,2015,38(1):66-69.DOI: 10.3760/cma.j.issn.1001-2036.2015.01.016. [30] 徐永清.小腿穿支皮瓣在中国的临床应用及进展[J].中华显微外科杂志,2020,43(6):521-534.DOI: 10.3760/cma.j.cn441206-20200527-00243. [31] 熊胜,巨积辉,金光哲,等.游离同侧多块小腿腓浅动脉穿支皮瓣修复手部多发创面效果观察[J].中华烧伤杂志,2019,35(9):655-660.DOI: 10.3760/cma.j.issn.1009-2587.2019.09.003. [32] 程贺云,张韬,巨积辉,等.Flow-through腓浅动脉皮瓣修复手指伴指掌侧固有动脉缺损创面[J].中华显微外科杂志,2021,44(4):369-373.DOI: 10.3760/cma.j.cn441206-20210111-00011. [33] 熊胜,巨积辉,金光哲,等. 彩超定位下游离腓浅动脉穿支皮瓣修复手足部创面[J]. 中华手外科杂志,2018,34(6):418-420. DOI: 10.3760/cma.j.issn.1005-054X.2018.06.007. [34] 石岩,何晓清,杨曦,等. CT血管造影检查结合三维重建辅助设计腓浅动脉穿支皮瓣修复手部创面的疗效[J]. 中华创伤杂志,2021,37(6):501-507. DOI: 10.3760/cma.j.cn501098-20210202-00105. [35] StoccoC,MurphyDC,GargiuloM,et al.Superficial peroneal nerve accessory artery (SPNAA) flap for head and neck reconstruction: a cadaveric anatomical study and retrospective case series review[J].J Plast Reconstr Aesthet Surg,2021,74(7):1524-1533.DOI: 10.1016/j.bjps.2020.11.012. [36] 张威凯,龚永清,尹绍猛,等. 游离腓浅动脉穿支双叶皮瓣修复双指皮肤缺损[J]. 中华手外科杂志,2016,32(5):397-398. DOI: 10.3760/cma.j.issn.1005-054X.2016.05.035. [37] 徐永清,何晓清,陈雪松,等. 手和足部创面修复时四种吻合血管的皮神经营养血管穿支皮瓣的选择[J]. 中华显微外科杂志,2020,43(4):331-337. DOI: 10.3760/cma.j.cn441206-20200218-00068. -









 下载:
下载:


 下载:
下载: